With age, you might have difficulty focusing on objects up close. You may become more sensitive to glare and have trouble adapting to different levels of light. Let’s look at some of the more common eye problems related to aging:
Genetic and clinical research has revealed a new form of macular dystrophy (A disease that causes central vision loss)
Researchers from the National Eye Institute (NEI) have identified a new disease that affects the macula, a small part of the light-sensing retina needed for sharp, central vision. Scientists report their findings on the novel macular dystrophy, which is yet to be named, in JAMA Ophthalmology. NEI is part of the National Institutes of Health.
Macular dystrophies are disorders that usually cause central visual loss because of mutations in several genes, including ABCA4, BEST1, PRPH2, and TIMP3.
For example, patients with Sorsby Fundus Dystrophy, a genetic eye disease specifically linked to TIMP3 variants, usually develop symptoms in adulthood. They often have sudden changes in visual acuity due to choroidal neovascularization- new, abnormal blood vessels that grow under the retina, leaking fluid and affecting vision.
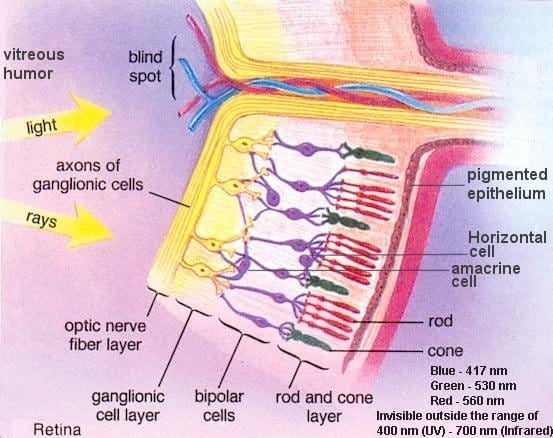
TIMP3 is a protein that helps regulate retinal blood flow and is secreted from the retinal pigment epithelium (RPE), a layer of tissue that nourishes and supports the retina’s light-sensing photoreceptors. All TIMP3 gene mutations reported are in the mature protein after it has been “cut” from RPE cells in a process called cleavage.
“We found it surprising that two patients had TIMP3 variants not in the mature protein, but in the short signal sequence the gene uses to ‘cut’ the protein from the cells. We showed these variants prevent cleavage, causing the protein to be stuck in the cell, likely leading to retinal pigment epithelium toxicity,” said Bin Guan, Ph.D., lead author.
The research team followed these findings with clinical evaluations and genetic testing of family members to verify that the two new TIMP3 variants are connected to this atypical maculopathy.
“Affected individuals had scotomas, or blind spots, and changes in their maculas indicative of disease, but, for now, they have preserved central vision and no choroidal neovascularization, unlike typical Sorsby Fundus Dystrophy,” said Cathy Cukras, M.D., Ph.D., a Lasker tenure-track investigator and medical retina specialist who clinically evaluated the patients.
NEI’s Ophthalmic Genomics Laboratory gathers and manages specimens and diagnostic data from patients who have been recruited into multiple studies within the NEI clinical program to facilitate research of rare eye diseases, including Sorsby Fundus Dystrophy.
“Discovering novel disease mechanisms, even in known genes like TIMP3, may help patients that have been looking for the correct diagnosis, and will hopefully lead to new therapies for them,” said Rob Hufnagel, M.D., Ph.D., senior author and director of the Ophthalmic Genomics Laboratory at NEI.
The study was funded by the NEI Intramural Research Program.
Summary: New research into octopus vision has led to a quick and easy test to help optometrists identify people who are at greater risk of macular degeneration, the leading cause of incurable sight loss.
New strategy for treating common retinal diseases shows promise A potential treatment based on a natural protein may offer broader benefits than existing drugs Scientists at Scripps Research have uncovered a potential new strategy for treating eye diseases that affect millions of people around the world, often resulting in blindness.
New insight on how people with retinal degenerative disease can maintain their night vision for a relatively long period of time has been published today in the open-access eLife journal. The study suggests that second-order neurons in the retina, which relay visual signals to the retinal ganglion cells that project into the brain, maintain their activity in response to photoreceptor degeneration to resist visual decline -- a process known as homeostatic plasticity.
When the eye isn't getting enough oxygen in the face of common conditions like premature birth or diabetes, it sets in motion a state of frenzied energy production that can ultimately result in blindness, and now scientists have identified new points where they may be able to calm the frenzy and instead enable recovery. In this high-energy environ, both the endothelial cells that will form new blood vessels in the retina -- which could improve oxygen levels -- and nearby microglia -- a type of macrophage that typically keeps watch over the retina -- prefer glycolysis as a means to turn glucose into their fuel.
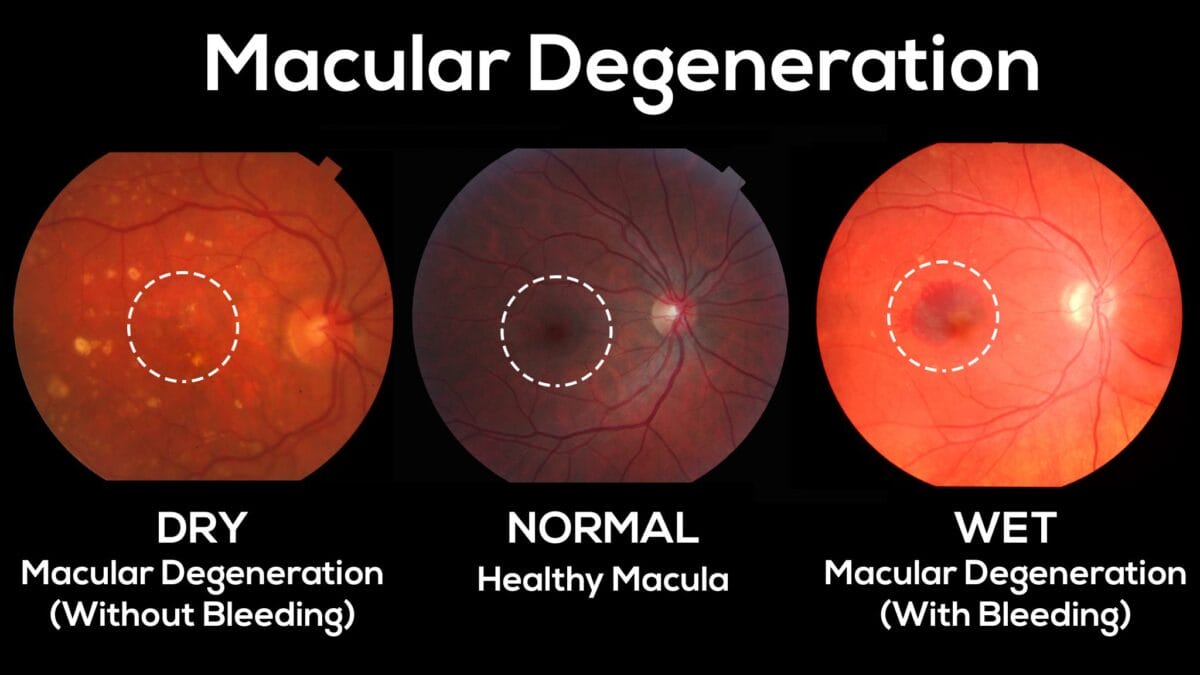
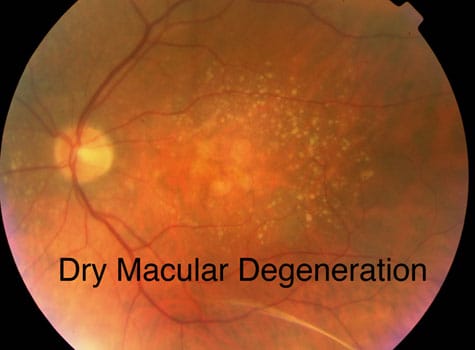
February Is Age-Related Macular Degeneration (AMD) / Low-Vision Awareness Month What is Macular Degeneration? Age-Related Macular Degeneration (AMD) is a relatively common eye condition. It is the leading cause of vision loss in adults 55 and over. It affects more than 10 million Americans – more than both glaucoma and cataracts combined.

Contact us
Call us
Visit us anytime
Goodrich Optical, 2450 Delhi Commerce Dr. Holt, MI 48842
Send us an email
About us
Subscribe
Sign up for our newsletter to receive all the latest eye health news as well as offers and discounts from Goodrich Optical.
Copyright © 2023 all rights reserved.