Experts from buck institute reveal a connection between diet, eye health and life expectancy in Drosophila. They find that the processes in the fly’s eye drive the ageing process. Previous studies have shown an association between eye disorders and poor health in humans.
My Optometrist recommended anti-fatigue lenses. Are they necessary? Anti-fatigue lenses are particularly helpful for close-up work. If you, like so many today, rely on your distance-only single-vision lenses, to see your screen clearly, anti-fatigue lenses may be the ideal solution for you.
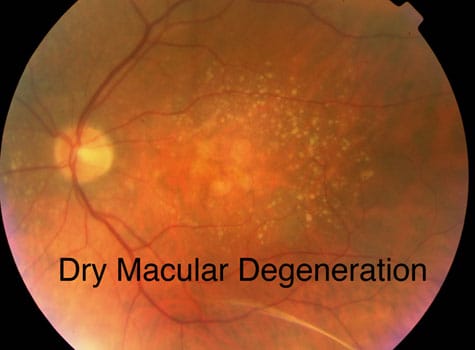
New insight on how people with retinal degenerative disease can maintain their night vision for a relatively long period of time has been published today in the open-access eLife journal. The study suggests that second-order neurons in the retina, which relay visual signals to the retinal ganglion cells that project into the brain, maintain their activity in response to photoreceptor degeneration to resist visual decline -- a process known as homeostatic plasticity.
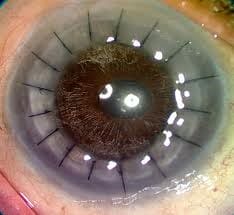
A new approach in ophthalmology that offers a revolutionary alternative to corneal transplantation has just been developed by researchers and clinicians in North America, Europe, and Oceania. The team was co-led by May Griffith, a researcher at Maisonneuve-Rosemont Hospital Research Centre, which is affiliated with Université de Montréal and is part of the CIUSSS de l'Est-de-l'Île-de-Montréal. The results of this multinational project have just been published in the journal Science Advances.
Cases of herpes zoster ophthalmicus tripled in 12-year time span, highest among older adults Source: Michigan Medicine - University of Michigan More Americans are being diagnosed with eye complications of shingles, but older adults can call the shots on whether they are protected from the painful rash that can cost them their eyesight.

Contact us
Call us
Visit us anytime
Goodrich Optical, 2450 Delhi Commerce Dr. Holt, MI 48842
Send us an email
About us
Subscribe
Sign up for our newsletter to receive all the latest eye health news as well as offers and discounts from Goodrich Optical.
Copyright © 2023 all rights reserved.