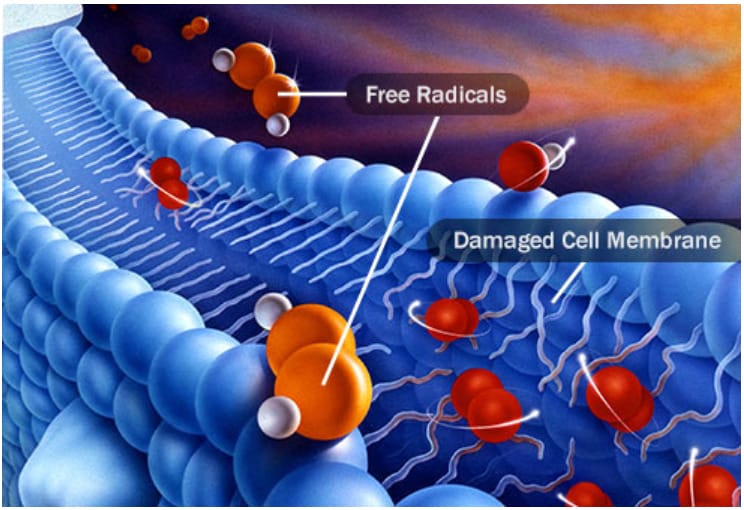
Antioxidants key to lowering risk of age-related cataracts A $5.7 billion global medical bill to restore sight for the estimated 45 million people with cataracts could be slashed in half by a diet rich in colorful fruits and vegetables, according to an international study.
A study has found that CBD -- a major chemical component in marijuana -- appears to increase the pressure inside the eye of mice, suggesting the use of the substance in the treatment of glaucoma may actually worsen the condition.
Supplementation Enhances Vision of Pre and Post Cataract Surgery Patients By Mihir Parikh, MD When vision is restored with successful cataract surgery and intraocular lens implantation, patients generally expect to have good vision for the rest of their lives. However, population studies do not necessarily support that assumption. A leading cause of permanent vision loss in the developed world is age-related macular degeneration (AMD), and the risk of AMD increases with advancing age.

Contact us
Call us
Visit us anytime
Goodrich Optical, 2450 Delhi Commerce Dr. Holt, MI 48842
Send us an email
About us
Subscribe
Sign up for our newsletter to receive all the latest eye health news as well as offers and discounts from Goodrich Optical.
Copyright © 2023 all rights reserved.