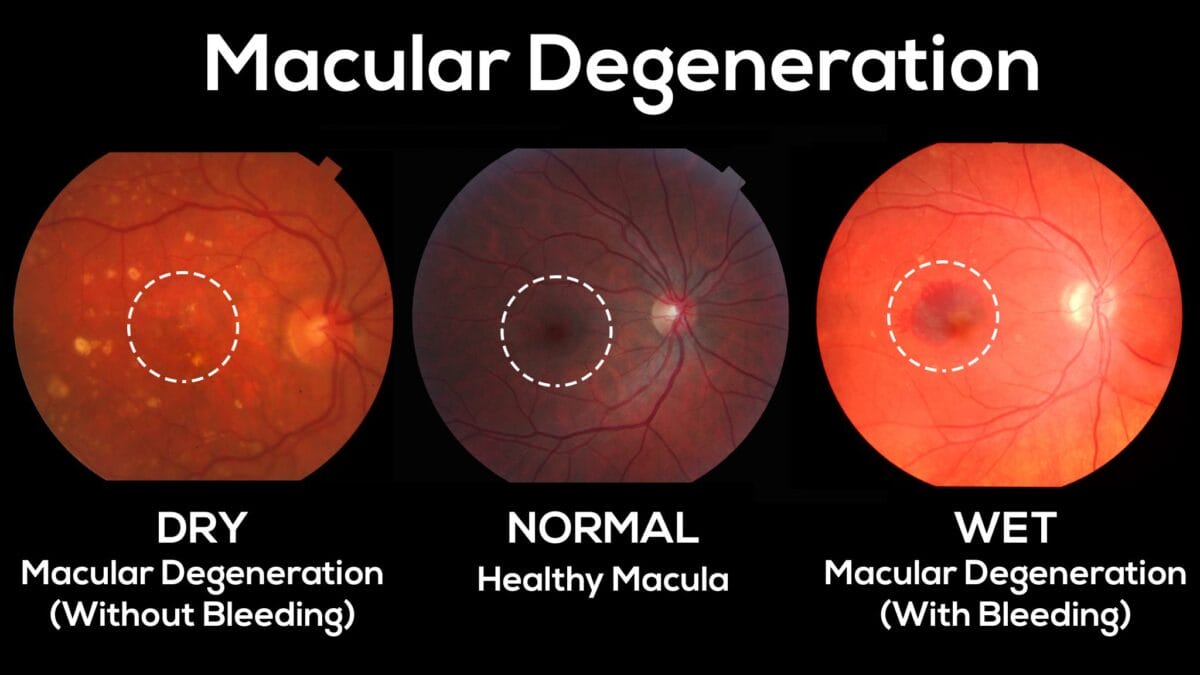
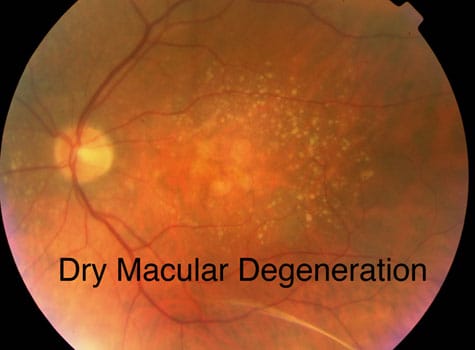
With age, you might have difficulty focusing on objects up close. You may become more sensitive to glare and have trouble adapting to different levels of light. Let’s look at some of the more common eye problems related to aging:
October is observed every year as Blindness Awareness Month, which focuses on understanding and supporting the problems faced by blind people. According to the World Health Organization, about 2.2 billion people worldwide suffer from visual impairment or blindness.
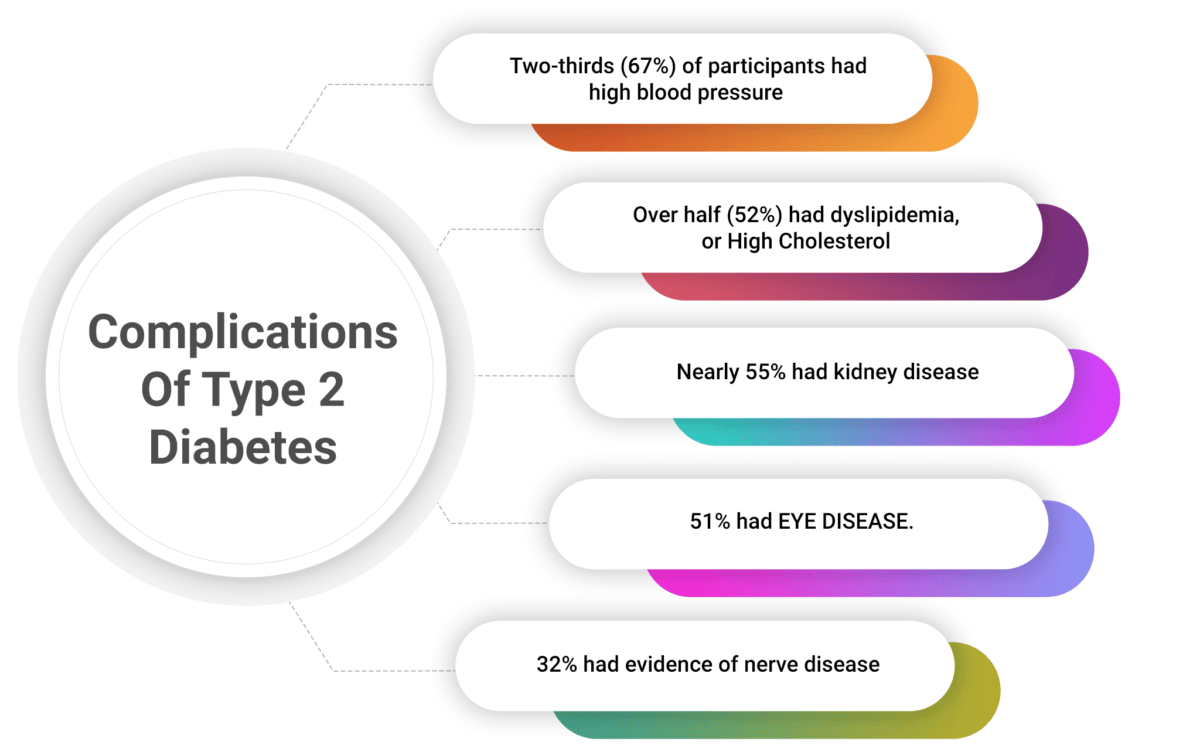
Phil Zeitler, MD, PhD, has been treating kids with type 2 diabetes for more than 20 years. He and a team of researchers published a paper in the TODAY2 Study in the New England Journal of Medicine on the long-term complications of type 2 diabetes. (TODAY stands for Treatment Options for type 2 Diabetes in Adolescents and Youth). The first phase of the study took place from 2004 -- 2011; phase two from 2011 -- 2020. Both studies involved more than 550 participants from across the country.
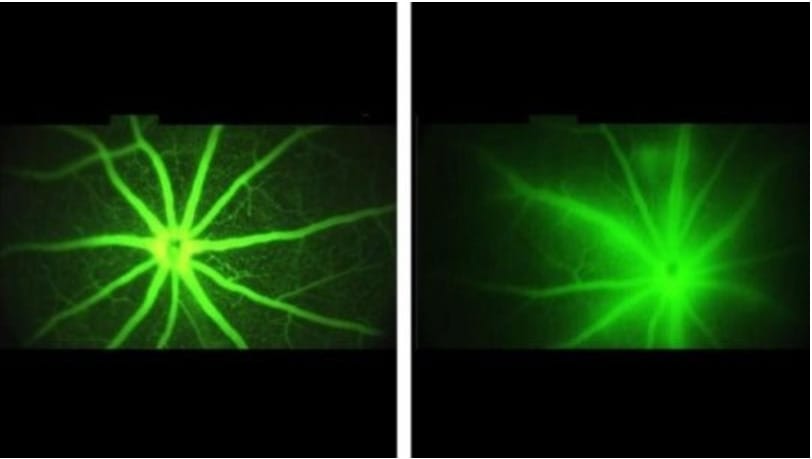
New strategy for treating common retinal diseases shows promise A potential treatment based on a natural protein may offer broader benefits than existing drugs Scientists at Scripps Research have uncovered a potential new strategy for treating eye diseases that affect millions of people around the world, often resulting in blindness.
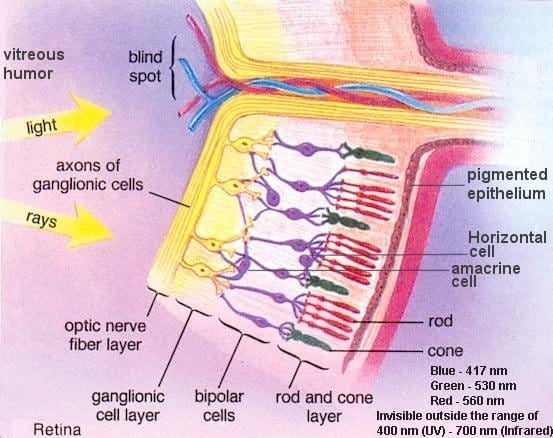
New insight on how people with retinal degenerative disease can maintain their night vision for a relatively long period of time has been published today in the open-access eLife journal. The study suggests that second-order neurons in the retina, which relay visual signals to the retinal ganglion cells that project into the brain, maintain their activity in response to photoreceptor degeneration to resist visual decline -- a process known as homeostatic plasticity.
When the eye isn't getting enough oxygen in the face of common conditions like premature birth or diabetes, it sets in motion a state of frenzied energy production that can ultimately result in blindness, and now scientists have identified new points where they may be able to calm the frenzy and instead enable recovery. In this high-energy environ, both the endothelial cells that will form new blood vessels in the retina -- which could improve oxygen levels -- and nearby microglia -- a type of macrophage that typically keeps watch over the retina -- prefer glycolysis as a means to turn glucose into their fuel.
In studies with lab-grown human cells and in mice, Johns Hopkins Medicine researchers have found that an experimental drug may be twice as good at fighting vision loss as previously thought. In studies with lab-grown human cells and in mice, Johns Hopkins Medicine researchers have found that an experimental drug may be twice as good at fighting vision loss as previously thought.
New Treatment could improve and prolong sight in those suffering vision loss Millions of Americans are progressively losing their sight as cells in their eyes deteriorate, but a new therapy developed by researchers at the University of California, Berkeley, could help prolong useful vision and delay total blindness.
Research shows that losing weight can help prevent or delay the onset of diabetes. While best practice for weight loss often includes decreasing or eliminating calories from alcohol, few studies examine whether people who undergo weight loss treatment report changes in alcohol intake and whether alcohol influences their weight loss.
Contact us
Call us
Visit us anytime
Goodrich Optical, 2450 Delhi Commerce Dr. Holt, MI 48842
Send us an email
About us
Subscribe
Sign up for our newsletter to receive all the latest eye health news as well as offers and discounts from Goodrich Optical.
Copyright © 2023 all rights reserved.