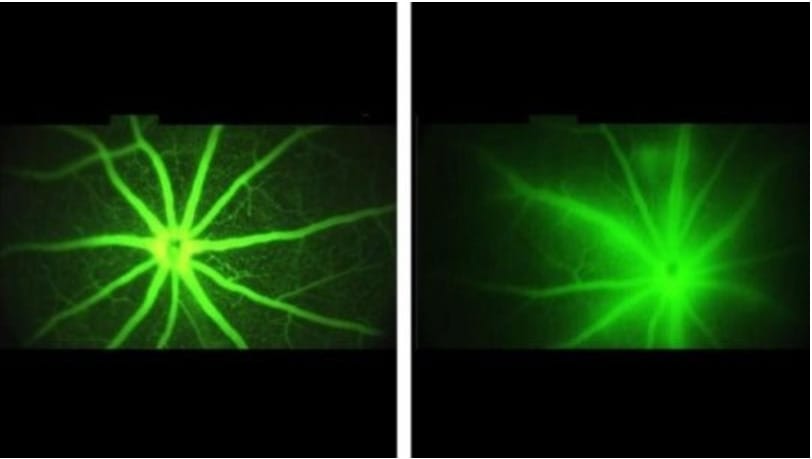
Reduced blood flow and impaired neurovascular coupling are well-known features of glaucoma, the main cause of non-curable blindness, affecting 80 million people worldwide in 2020. The mechanisms behind these abnormalities are now known, thanks to new research by a team led by Adriana Di Polo, professor of neuroscience and ophthalmology at Université de Montréal. The findings by Luis Alarcon-Martinez and Yukihiro Shiga, both post-doctoral fellows in Di Polo’s laboratory and co-authors of the study, reveal that nanotubes connecting pericytes are damaged in glaucoma leading to neurovascular failures.
Changing environmental factors as well as changing gene-environment interactions could be to blame for increasing rates of myopia, also known as nearsightedness or shortsightedness.
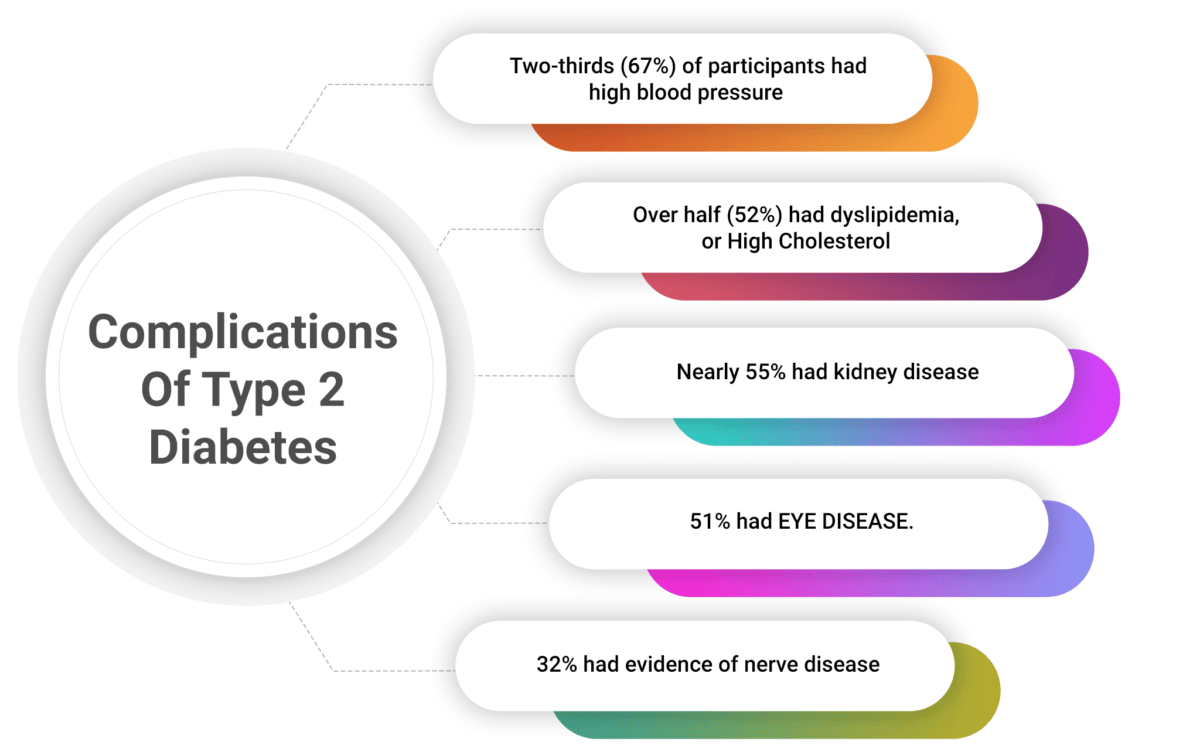
Phil Zeitler, MD, PhD, has been treating kids with type 2 diabetes for more than 20 years. He and a team of researchers published a paper in the TODAY2 Study in the New England Journal of Medicine on the long-term complications of type 2 diabetes. (TODAY stands for Treatment Options for type 2 Diabetes in Adolescents and Youth). The first phase of the study took place from 2004 -- 2011; phase two from 2011 -- 2020. Both studies involved more than 550 participants from across the country.
New insight on how people with retinal degenerative disease can maintain their night vision for a relatively long period of time has been published today in the open-access eLife journal. The study suggests that second-order neurons in the retina, which relay visual signals to the retinal ganglion cells that project into the brain, maintain their activity in response to photoreceptor degeneration to resist visual decline -- a process known as homeostatic plasticity.
The Digital Gap Between Rich and Poor Kids Is Not What We Expected America’s public schools are still promoting devices with screens — even offering digital-only preschools while the rich are banning screens from class altogether.
Eyes hold clues for treating severe autism more effectively Vocabulary tests for individuals with the severest forms of autism spectrum disorder, or ASD, are notoriously inaccurate. They commonly ask the test-taker to point to an illustration after hearing a spoken word, measuring the ability to understand and perform a task as much as word knowledge.
Cases of herpes zoster ophthalmicus tripled in 12-year time span, highest among older adults Source: Michigan Medicine - University of Michigan More Americans are being diagnosed with eye complications of shingles, but older adults can call the shots on whether they are protected from the painful rash that can cost them their eyesight.
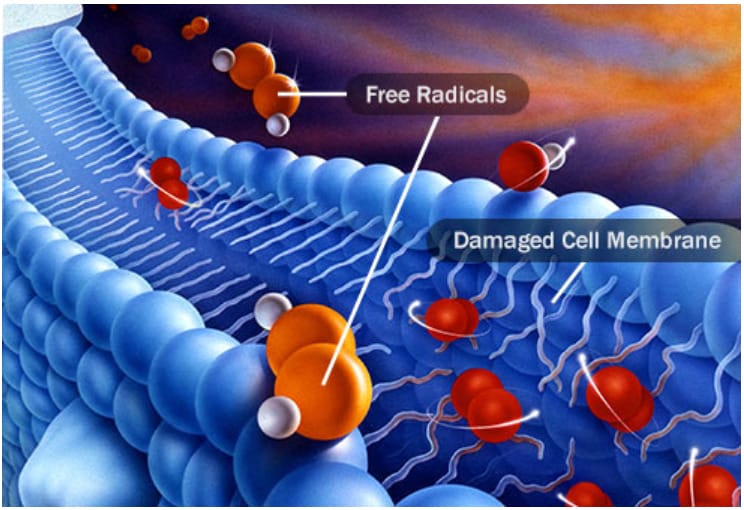
Antioxidants key to lowering risk of age-related cataracts A $5.7 billion global medical bill to restore sight for the estimated 45 million people with cataracts could be slashed in half by a diet rich in colorful fruits and vegetables, according to an international study.
In studies with lab-grown human cells and in mice, Johns Hopkins Medicine researchers have found that an experimental drug may be twice as good at fighting vision loss as previously thought. In studies with lab-grown human cells and in mice, Johns Hopkins Medicine researchers have found that an experimental drug may be twice as good at fighting vision loss as previously thought.
New Treatment could improve and prolong sight in those suffering vision loss Millions of Americans are progressively losing their sight as cells in their eyes deteriorate, but a new therapy developed by researchers at the University of California, Berkeley, could help prolong useful vision and delay total blindness.

Contact us
Call us
Visit us anytime
Goodrich Optical, 2450 Delhi Commerce Dr. Holt, MI 48842
Send us an email
About us
Subscribe
Sign up for our newsletter to receive all the latest eye health news as well as offers and discounts from Goodrich Optical.
Copyright © 2023 all rights reserved.